Many authors address concerns about having safer sex during the COVID-19 crisis. Most advice focuses on enhancing your ability to enjoy self-pleasure. Others suggest experimenting with virtual ways to engage. While self-love remains an important thing, sometimes touching yourself just doesn’t cut it. And virtual love-making doesn’t work for everyone either.
Early in the pandemic, the universal advice was keep to yourself. However, many single folks live alone and get their needs for intimacy met through dating. They may not have an exclusive partner right now. Those who enjoy open relationships often do not live with all their partners. Sex educator Tristan Taormino stated, “polyamory is canceled unless you live with all your partners.” While keeping distance for eight weeks might be manageable, evidence points to the unsustainability of that strategy. So now what?
Safer Routes to Getting Your Needs Met
Empowering advice that provides guidance for expanding your intimate circle may be hard to find. The sex-negative culture you live in minimizes the importance of intimacy and physical pleasure. Experts tend to assume that sexual risks are bigger than they actually are. Yet, it’s important to be informed about risk. For example, coronavirus has been found in fecal material, so make sure you’re extra careful about anal play.
You get to determine what your needs are. You may feel pretty risk averse. The need to do everything in your power to stay healthy comes first. Perhaps you feel torn between limiting your exposure and the intense longing in your body for human contact. You might be the person who’s pretty cool with exposure concerns, and yet your partner lives with someone who is immunocompromised.
All of these unique scenarios require different responses. Your choices reflect what matters to you, feels significant to you and resonates with your body. The decisions you make around your risk tolerance and need for human connection are yours. And yet, they impact and interact with the needs of others. That means open, honest, complete communication and clear agreements with those around you must happen. That’s the ethical imperative – not whether you choose to shelter-in-place until the end of the year.
You might be feeling a bit intimidated by this idea. Honest and direct communication is challenging. It can feel uncomfortable. However, leaning into this discomfort enables you to practice doing it right. It leads to acting in an ethical manner that supports the common good. In the rest of this post, I’ll share frameworks that you can use and examples from the consensually non-monogamous (CNM) folk I work with.
How to Communicate with Others
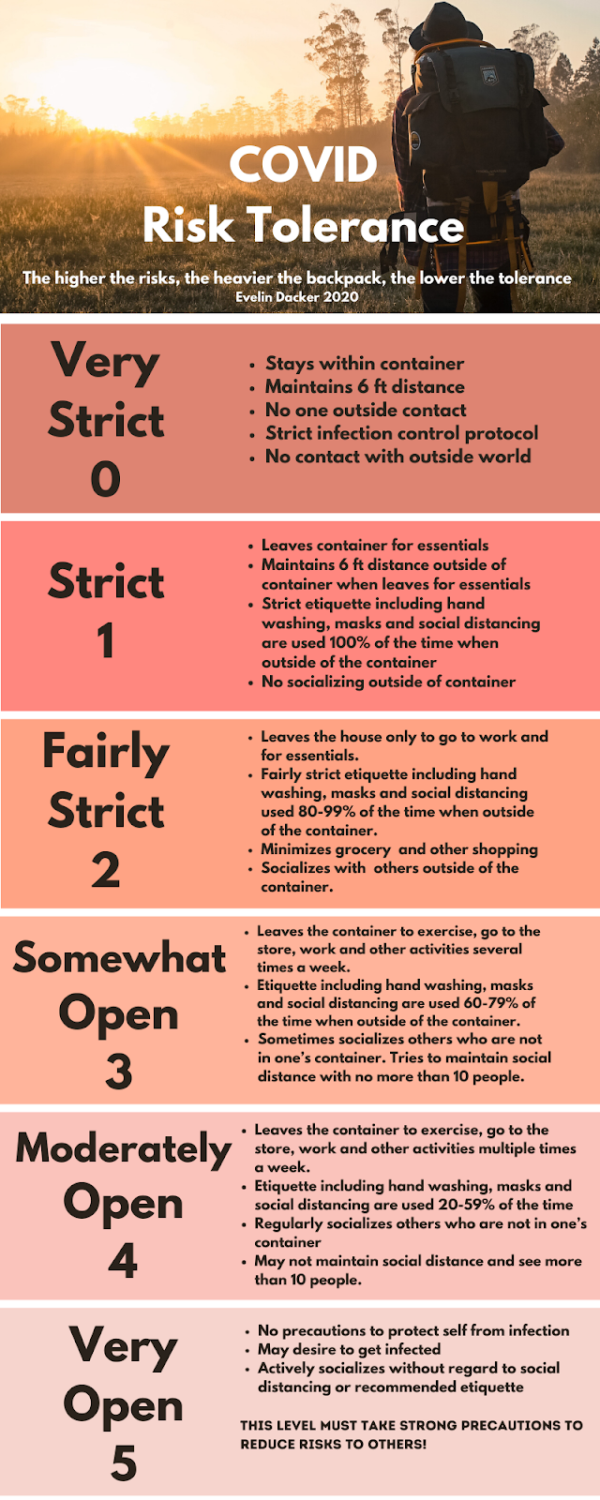
First off, you need language. You need a way to clearly, easily communicate with those around you about the steps you’re taking to stay healthy. Dr. Evelin Dacker provides a great framework for this conversation in her article COVID CARE: A Way Forward (another piece you should read).
This graphic from Dr. Dacker breaks down the ways you and others may choose to change behavior to mitigate risk. You get to choose what level of risk you are willing to tolerate. Everyone else around you does to. Next, you have to talk about it.
Steps to prepare for the conversation
- Consider your own health risks
- Consider the health risks of others in your household
- Decide where your risk tolerance falls on this chart
- Communicate with others who you do not live with before you take off your mask and get close
- Regularly update your understanding with everyone you have contact with
- In some ways, this approach may seem familiar to you.
Use Your Existing Safer Sex Skills in a New Way
Likewise, this approach builds on safer sex practices that developed during the AIDS crisis. As Gregg Gonsalves, a public health researcher at Yale, says, “There are ways to manage risk, without putting unreasonable expectations on people over long periods of time. This is why back in the early days of HIV, we invented safer sex.”
Hopefully, practicing safer sex comes naturally to you. You remember to bring and use condoms and other barriers. Regular STI testing seems routine to you. Talking with your partners about safer sex concerns – no big deal.
So thanks to coronavirus, the safer sex Elevator Speech that you’ve been using before intimacy applies to all social interactions now.
For some of you, this direct conversation is likely new and feels uncomfortable. Feeling uncomfortable may be something you prefer to avoid. However, if you lean into that discomfort, then you will discover this type of communication enhances your options and eases anxiety.
Maybe you or someone you know practices polyamory. That is to say, if you do, then you have some informal expertise to draw from. See, folks in open relationships regularly navigate the tension of known unknowns and differences in risk tolerance related to STIs. Folks who regularly engage with multiple sex partners, from an ethical place, use agreements and rules to help protect their health all the time. And many of them are leading the way in navigating this pandemic context.
Build Your Intimacy Container with Others
One practice to consider is building a “container” or a “germacule.” Objectively speaking, anyone you share indoor air with regularly is part of your container. So anyone you live with and the residents of other households are members of your container, scientifically speaking.
Ideologically speaking, your germacule should consist of the folks who are willing to take similar precautions and communicate about any deviations from those agreements. So if your risk tolerance is around a strictness level 2, then you will want to build a container with other people who are also around a level 2 or 3. This means keeping a social distance from folks outside your germacule.
Safer Sex Role Models
Some polyamorous individuals use the two-week quarantine buffer as a way to move between different containers over time. For example, one of my clients lives with an immunocompromised person who is at level 1 or 2. Other desired members of their germacule prefer level 3 or 4. And their personal risk tolerance is about a 3. This client enjoys all these people (over time) by using a two-week rotating schedule. During one two-week period they spend time with the person who needs a stricter level of precaution, and during the other two-week period they can hang out with everyone else.
Another polyamorous client of mine finds comfort in knowing where her “dead-ends” are. Because her container is well-defined, she knows the extent of who she’s had direct contact with, and who they’ve had direct contact with, at any given time. This knowledge means she can do her own contact tracing if anyone in her container gets sick. Many of my clients talk about feeling positive about working on these agreements and respecting others’ risk tolerances.
If you’re dating around, then consider staying socially distant for casual dates. Once you’ve gotten close to someone, then consider waiting two weeks before you hook up with someone else. Another client of mine finds this strategy is working well.
This weird moment in history provides an interesting opportunity to experiment with getting to know people in a wide variety of formats. You can take advantage of all of them. You’re likely to find, as the pioneers of safer sex learned, that doing so improves your relationships. It will deepen your intimate relationships, improve your self-awareness, and increase your ability to discuss your needs and boundaries outside the bedroom as well. And imagine the kind of world we’d have coming out of the pandemic if we all did that?